Biological Effects of Radiation Part 2: Radiosensitivity (ARRT Registry Review)
Nov 22, 2025

Radiation's interaction with living tissue is not uniform — some cells and systems are more vulnerable than others. This property, known as radiosensitivity, is central to understanding diagnostic imaging, radiation therapy, and radiation protection principles. For those preparing for the ARRT Registry, mastering this concept is essential.
In this second part of our blog series on the biological effects of radiation, we will explore the factors that influence radiosensitivity, including dose-response relationships, relative tissue responses, cell survival (LD50), and the oxygen effect. We’ll also highlight how these concepts tie into energy transfer mechanisms such as LET and RBE, providing clinical and conceptual clarity.
1. Dose-Response Relationships: How Much Is Too Much?
Radiation dose-response relationships describe the correlation between the amount of radiation absorbed and the biological response that results. These curves are foundational to understanding radiation risk assessment and treatment planning, especially in differentiating between stochastic and deterministic effects.
-
Stochastic effects (e.g., cancer, genetic mutations) are random and probabilistic. They follow a linear non-threshold (LNT) model, meaning even the smallest dose carries some risk. This model underlies most radiation safety guidelines — implying no dose is completely safe.
-
Deterministic effects (e.g., skin erythema, cataracts, acute radiation syndrome) have a threshold dose. Once surpassed, the severity of the effect increases with dose. These follow linear threshold or non-linear threshold models.
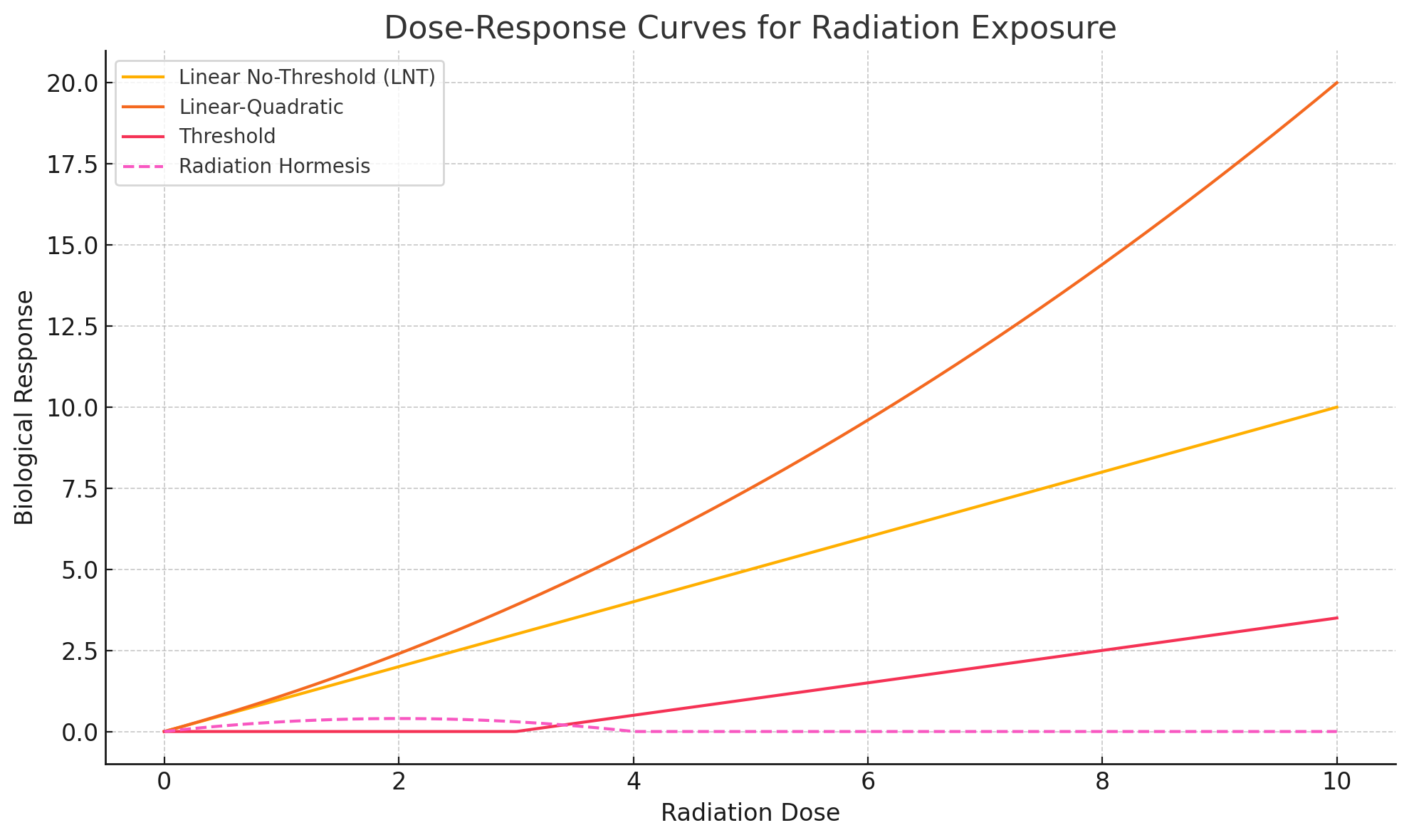
The ARRT may ask you to identify which conditions follow which curve:
-
Linear Non-Threshold: Leukemia, carcinogenesis, genetic mutations
-
Linear Threshold: Acute radiation syndrome, hematologic depression
-
Non-linear Threshold: Skin effects, cataracts, sterility
2. Relative Tissue Radiosensitivity: The LET and RBE Connection
Not all types of radiation cause the same amount of biological damage — and not all tissues are equally vulnerable. This variability is explained by concepts like Linear Energy Transfer (LET) and Relative Biologic Effectiveness (RBE).
-
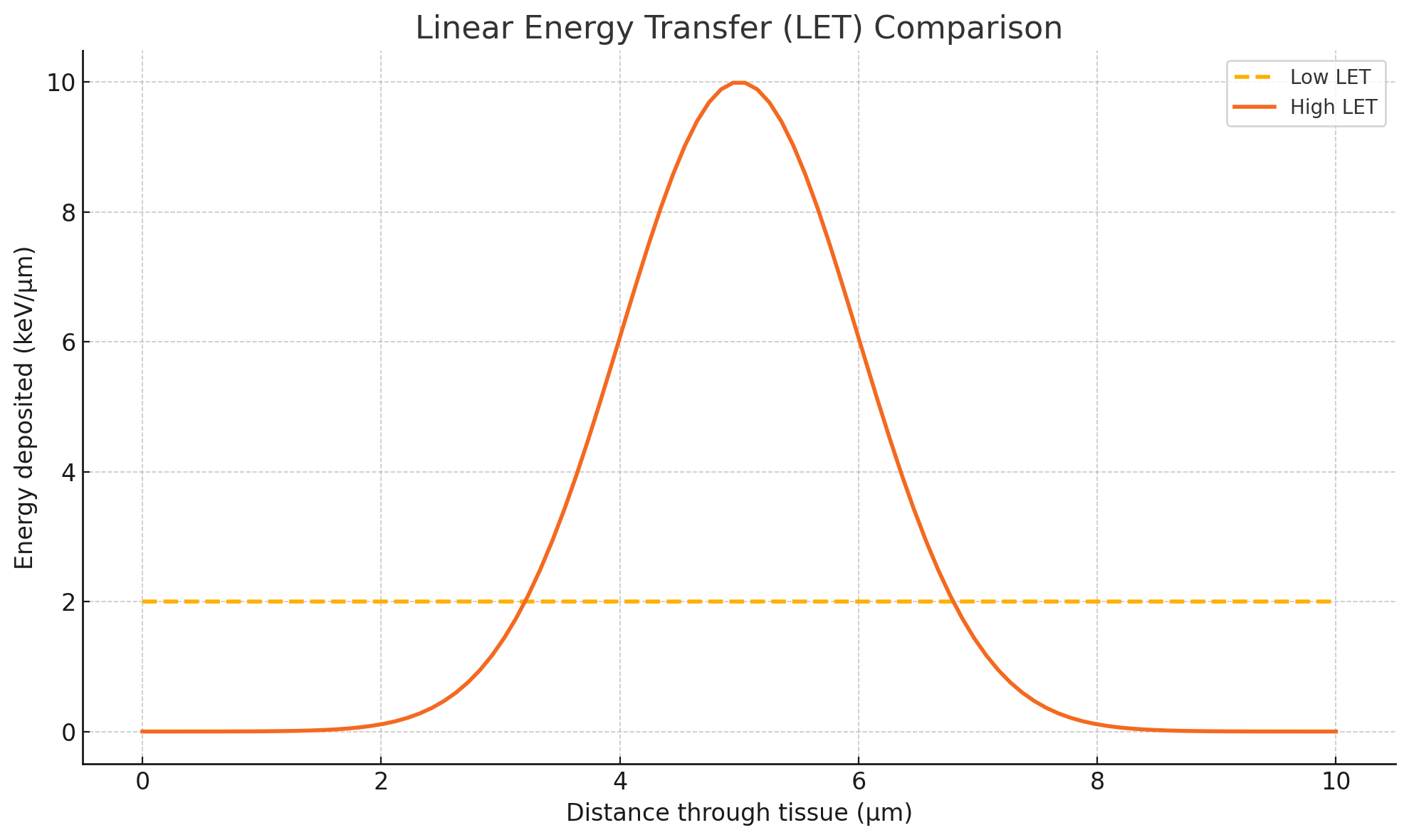
LET measures how much energy is deposited along the path of radiation through tissue (in keV/μm).
-
Low LET radiation (e.g., x-rays, gamma rays) is sparsely ionizing and spreads energy over longer tracks.
-
High LET radiation (e.g., alpha particles, neutrons) is densely ionizing and deposits more energy locally, causing greater damage per unit of dose.
-
-
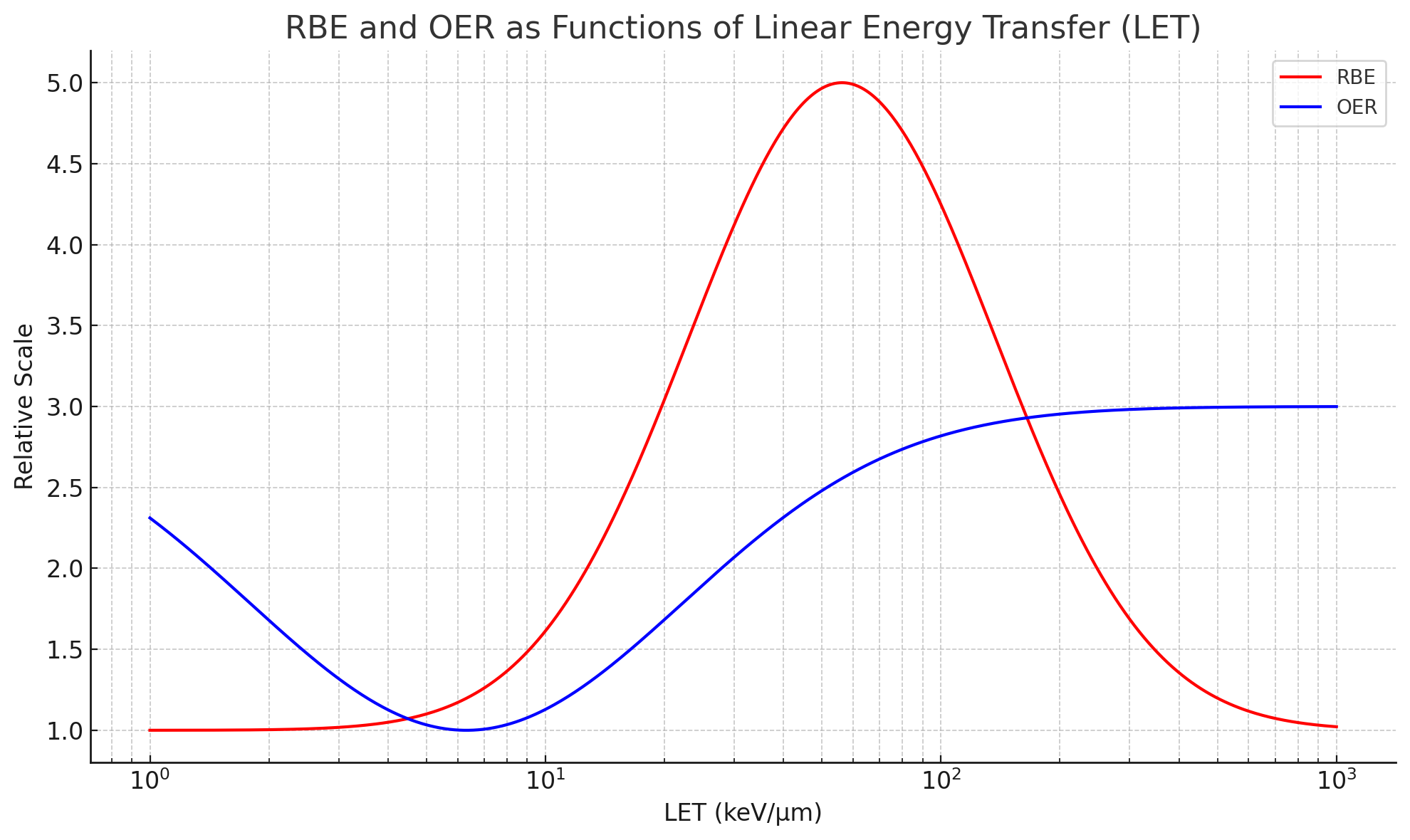
RBE quantifies how biologically damaging a type of radiation is compared to a standard, typically 250 keV x-rays.
-
Higher LET radiation generally has a higher RBE.
-
RBE increases with LET up to a point, after which it decreases due to overkill — the energy is too intense to cause further effect.
-
-
Cellular Impact: High LET radiation is more effective at causing double-strand DNA breaks, which are harder for cells to repair. This is especially critical in cancer therapy using heavy ions.
3. Radiosensitivity by Tissue Type: The Law of Bergonié and Tribondeau
Established in 1906, the Law of Bergonié and Tribondeau states that radiosensitivity is directly proportional to a cell’s reproductive activity and inversely proportional to its level of differentiation.
In simple terms:
-
Immature, undifferentiated, and rapidly dividing cells are the most radiosensitive.
-
Highly specialized, non-dividing cells are more radioresistant.
High Radiosensitivity (Most Sensitive)
-
Lymphocytes (most sensitive blood cell)
-
Spermatogonia (immature male germ cells)
-
Intestinal crypt cells (precursors to epithelial cells)
-
Erythroblasts (immature red blood cells)
Intermediate Radiosensitivity
-
Endothelial cells (lining of blood vessels)
-
Osteoblasts (bone-building cells)
-
Fibroblasts (collagen-producing connective tissue cells)
Low Radiosensitivity (Most Resistant)
-
Muscle cells (myocytes)
-
Nerve cells (neurons)
The cell cycle also influences sensitivity. The most vulnerable phases are:
-
G1 to early S phase (pre-DNA synthesis)
-
Metaphase of mitosis, when chromosomes align and are most susceptible to damage
4. Cell Survival and Recovery: Understanding LD50
When evaluating the biological impact of radiation, one key metric is LD50, or Lethal Dose 50, which identifies the dose required to kill 50% of a population within a set time.
-
LD50/30: Refers to the radiation dose that would kill 50% of a population within 30 days. This is commonly used in animal studies.
-
LD50/60: More applicable to humans, this measures survival over a 60-day period post-exposure.
In humans, the LD50/60 is approximately 3.2–4.5 Gy without medical intervention. With supportive care (e.g., antibiotics, hydration, bone marrow transplants), survival can extend to exposures up to 8.5 Gy or more, though long-term recovery may still be impaired.
Why is this important for the ARRT exam? It helps differentiate between deterministic thresholds and survival potential, which is crucial in emergency radiology, radiation accidents, or therapeutic overexposures.
Radiation therapy, which delivers high localized doses, uses knowledge of cell kill curves and recovery time to maximize tumor destruction while minimizing harm to normal tissues. This is achieved through dose fractionation — breaking total radiation into multiple small doses over time, allowing normal tissues to repair and survive.
5. The Oxygen Effect: Why Air Matters
A crucial modifier of radiosensitivity is oxygen. The oxygen effect explains why cells irradiated in an oxygenated environment are more sensitive than those in hypoxic or anoxic conditions.
-
Oxygen Enhancement Ratio (OER) quantifies this effect:
Typical OER values for x-rays are 2.5 to 3, meaning cells are up to three times more sensitive in the presence of oxygen.
-
As LET increases, OER decreases — high-LET radiation (e.g., alpha particles) is less affected by oxygen.
-
Low-LET radiation (e.g., x-rays) shows greater radiosensitization in the presence of oxygen.
Clinical Relevance
-
Tumors with poor blood supply (hypoxic) are often more radioresistant, making them harder to treat with standard x-rays.
-
Radiation oncologists may use hyperbaric oxygen therapy or chemical radiosensitizers to enhance treatment efficacy.
Understanding this relationship empowers professionals to adjust treatment strategies — maximizing cell kill in tumors while sparing normal tissue.
6. LET, RBE, and OER in Perspective
To synthesize what we’ve covered:
-
LET: Describes energy deposition. High LET = more localized damage.
-
RBE: Compares the biological effectiveness of different radiation types. High LET radiation has a higher RBE.
-
OER: Quantifies the role of oxygen in radiosensitivity. Low LET radiation has a higher OER.
These three factors interrelate, especially in radiation therapy planning:
-
High LET radiation: Preferred when targeting hypoxic tumors, where oxygen effect is minimal.
-
Low LET radiation: Highly effective in oxygen-rich environments due to a stronger OER.
These variables also inform how radiation is fractionated or protracted in clinical settings to minimize late effects and allow normal tissue recovery.
7. Radiosensitivity and Cell Cycle Phases
Cells are not equally sensitive throughout their lifecycle. Radiosensitivity peaks at specific cell cycle phases:
-
Most Radiosensitive:
-
G1 → Early S Phase: The cell prepares for DNA replication — any damage here can disrupt the cycle.
-
Metaphase: Chromosomes align, making them fully exposed and vulnerable.
-
-
Most Radioresistant:
-
Late S Phase: The cell has already duplicated its DNA and prepares for division, often with protective mechanisms activated.
-
This pattern is vital in cancer treatment, as tumors with rapid turnover are targeted more efficiently when their cells are in radiosensitive phases.
8. Human Tissue Radiosensitivity: From Blood to Brain
Not all human tissues respond to radiation in the same way. Their radiosensitivity depends on cell turnover rate, specialization, and metabolic activity, aligning with the principles of the Bergonié and Tribondeau law.
Most Radiosensitive Tissues
-
Blood cells, especially lymphocytes, are extremely radiosensitive. They are often the first to decline after radiation exposure, making hematopoietic suppression an early marker of overexposure.
-
Reproductive cells:
-
Spermatogonia (immature sperm cells) are more sensitive than spermatocytes.
-
Oogonia (female germ cells) also demonstrate high sensitivity, though females are born with all their eggs, limiting regeneration.
-
-
Epithelial and crypt cells, especially those lining the gastrointestinal tract, are vulnerable due to rapid mitosis and constant renewal.
Intermediately Sensitive Tissues
-
Endothelial cells, fibroblasts, osteoblasts, and spermatids fall into this category. While more differentiated, they still retain some proliferative capacity.
Least Radiosensitive Tissues
-
Muscle cells (myocytes) and nerve cells (neurons) are among the most radioresistant. Their specialization and non-dividing nature make them less vulnerable to DNA-damaging effects of radiation.
This ranking matters greatly in both diagnostic imaging and radiation therapy:
-
Shielding and dose optimization are critical when imaging areas like the abdomen, where radiosensitive tissues reside.
-
In radiation oncology, beam direction and dose planning aim to avoid long-term harm to muscle and nerve tissues.
9. Practical Applications: Fractionation, Protraction, and Recovery
Radiation therapy doesn't just rely on high doses; it leverages time and biology. The principles of dose fractionation and protraction play a crucial role in minimizing damage to healthy tissue:
-
Fractionation: Dividing the total radiation dose into smaller, individual doses over days or weeks.
-
Protraction: Spreading the total dose out over a longer continuous time at a lower rate.
Both strategies allow normal cells time to repair, whereas tumor cells — often less efficient at DNA repair — accumulate lethal damage.
This principle reflects in:
-
Higher recovery and survival rates post-radiation.
-
Reduction in late tissue effects such as fibrosis or necrosis.
-
Enhanced therapeutic outcomes, especially in cancers with mixed oxygenation and varied cell cycle phases.
10. Test-Ready Recap for ARRT Candidates
Let’s summarize the key takeaways that will help you ace the ARRT Registry section on radiosensitivity:
-
Dose-Response Relationships
-
LNT model applies to cancer and genetic effects.
-
Threshold models apply to skin effects, cataracts, and acute radiation syndrome.
-
-
Radiosensitivity by Cell Type
-
High: lymphocytes, stem cells, germ cells
-
Intermediate: endothelial cells, osteoblasts
-
Low: muscle and nerve cells
-
-
LET, RBE, OER
-
High LET = High RBE, Low OER
-
Low LET = Lower RBE, Higher OER
-
Oxygen increases radiosensitivity, especially for x-rays
-
-
Cell Cycle Sensitivity
-
Most sensitive during G1 to early S phase and metaphase
-
-
LD50 Values
-
LD50/60 ~ 3.2–4.5 Gy (without treatment)
-
Higher doses require intensive care to survive
-
-
Clinical Application
-
Use fractionation/protraction for tissue recovery
-
Target oxygenated tumor regions for maximum effect
-
Prioritize shielding for radiosensitive tissues
-
Conclusion: Radiosensitivity in Perspective
Understanding radiosensitivity is more than a testing requirement — it's a lens into cellular vulnerability, treatment precision, and patient safety. Whether you're administering a chest x-ray or planning a radiation treatment field, these principles guide every exposure.
Mastering the biology behind radiation's effects will not only improve your test scores — it will enhance your clinical judgment and patient care.
Want to take a deeper dive?
Consider joining hundreds of students in the 21 Day Registry Review Challenge, a self-paced course taught by over 42 instructors covering everything you need to know for the ARRT registry exam.
Click here to learn more: https://www.radtechregistry.com/store
Stay connected with news and updates!
Join our mailing list to receive the latest tips, tricks and insights to help you pass your registry!
We hate SPAM. We will never sell your information, for any reason.

